Supporting Premenstrual Syndrome with Herbal Medicine
Wherever you may be on your journey toward optimal health and well-being, I hope you know that there are a wide variety of incredibly powerful and helpful herbs to consider safely integrating into your lifestyle that can help you to feel your level best and balance the debilitating effects of PMS.
Supporting PMS with Herbal Medicine
Herbal medicine is a powerful holistic tool for supporting premenstrual syndrome (PMS), a common disorder affecting women during the seven-to-ten-day period prior to menstruation. Symptoms vary widely and are so numerous that diagnosis can frequently be difficult. PMS is diagnosed on the basis of symptoms beyond normal cyclical menstrual body changes that cause disturbance in a woman’s life. This includes hormonal and/or chemical changes that cause debilitating symptoms. It occurs during the proliferative or luteal phase of menses when progesterone and estrogen levels are relatively high.
Several of the etiological factors identified for primary PMS include: excess estrogen, fluid retention, progesterone deficiency, magnesium deficiency, hypoglycemia, decreased production of prostaglandin E1, increased production of other prostaglandins and increased prolactin levels. PMS has over 200 associated symptoms, including any or all of the following: abdominal pain, acne, anxiety, breast swelling and tenderness, cramps, depression, dysphoria, fainting spells, fatigue, food cravings, headaches, insomnia, irritability, joint pain, nervousness, skin eruptions, water retention, personality changes like mood swings, anger outbursts, tension, violence and even thoughts of suicide.
Herbal Actions to Support PMS
Uterine Tonics provide a nourishing, toning and strengthening effects on the function and tissue of the female reproductive system. This herbal action is very beneficial for reducing and preventing PMS symptoms (Hoffman, 2003). Uterine tonics can also help to restore prenatal reproductive essence or vitality lost through menstruation, chronic stress, or illness (Reid, 1995).
Hormonal Normalizers provide an herbal action that directly impacts and naturally stabilizes the levels of hormones in the body. They help with regulating excess estrogen, progesterone deficiency, and other hormonal instability to more balanced levels (Hoffman, 2003).
Antispasmodics assist in preventing or lessening muscular spasms, cramps, and tension. They can even ease psychological tension and instability as well, like the reproductive antispasmodics Viburnum opulus (cramp bark) and V. prunifolium (black haw) (Hoffman, 2003).
Uterine Demulcents aid in soothing and toning inflamed tissue. They aid in reducing the manifestation of inflammatory PMS symptoms like cramps, joint pain, water retention, breast swelling, and tension (Hoffman, 2003).
Hepatics aid the functioning of the liver, along with all cholagogues and bitters. They do this by toning, strengthening and increasing the flow of bile. This herbal action helps with regulating hormonal balance and can also have a marked effect on supporting the muscles of the uterus.
Additionally, the herbal anti-inflammatory, nervine, emmenagogue, uterine demulcent, uterine astringent and yin balancing or tonifying actions can also be very supportive. I often bring in all of the above-mentioned herbal actions into my custom clinical herbal formulas when individually indicated for a person’s unique constitution and healthcare needs.
Specific Herbs to Support Targeted Herbal Actions
Hormonal Normalizers
Vitex agnus-castus, chaste tree berry
Paeonia lactiflora, peony
Salvia officinialis, sage
Dioscorea villosa, wild yam
Glycyrrhiza glabra, licorice
Cnicus benedictus, blessed thistle
Angelica sinensis, dong quai
Uterine Tonics
Cimicifuga racemosa, black cohosh
Mitchella repens, partridgeberry
Rubus idaeus, raspberry leaf
Caulophyllum thalictroides, blue cohosh
Tribulus terrestris, gokshura
Lepedium meyenii, maca
Angelica sinensis, dong quai
Uterine Demulcents
Caulophyllum thalictroides, blue cohosh
Asparagus racemosus, shatavari
Antispasmodic
Viburnum opulus, cramp bark
Viburnum prunifolium, black haw
Dioscorea villosa, wild yam
Valeriana officinalis, valerian
Scutellaria lateriflora, skullcap
Emmenagogues
Achillea millefolium, yarrow
Artemisia vulgaris, mugwort|
Mitchella repens, partridgeberry
Rubus idaeus, raspberry
Vitex agnus-castus, chaste tree berry
Hepatics
Achillea millefolium, yarrow
Agrimonia eupatoria, agrimony
Curcuma longa, turmeric
Mahonia aquifolium, Oregon grape
Zanthoxylum americanum, prickly ash
Yin Balancing/Tonifying
Rehmannia glutinosa
Lycium chinensis, Chinese wolfberry
Dioscorea japonica, East Asian mountain yam
Paeonia suffruticosa, tree peony
Alisma orientalis, Asian water plantain
A Closer Look at Several PMS-Supporting Herbs
Cramp Bark (Viburnum opulus) longstanding reputation as well as modern use for relaxing muscular tension and spasm in voluntary muscles as well as uterine muscles problems; also indicated for painful menstrual cramps, endometriosis, chronic pelvic pain and dysmenorrhea; herbal actions include nervine, anti-inflammatory and emmenagogue
Corydalis tuber (Corydalis yanhusuo) indicated for nociceptive pain, spasmodic dysmenorrhea and endometriosis; herbal actions include antispasmodic, analgesic, mild sedative, hypnotic, anxiolytic; also referenced in the Handbook of Chinese Medicine for traditional use supporting the liver and spleen meridians, and regulating the circulation of chi and blood flow
Black Cohosh rhizome with rootlet (Actaea racemosa) longstanding Native American application for female reproductive problems, pain during childbirth, dysmenorrhea and uterine colic; traditional Cherokee use as a plant medicine of the North for relaxing the nerves, settling the heart and spirit; eases physical and mental changes associated with perimenopause and menopause as well as hormonal deficits as a result of hysterectomy or ovariectomy; a treatment for hot flashes, insomnia, headache, irritability, depressive moods and spasmodic dysmenorrhea; herbal actions include antispasmodic, anti-inflammatory, alterative, nervine, emmenagogue, hormonal normalizer for the female reproductive system and sedative
Wild Yam rhizome (Dioscorea villosa) extensive traditional Indigenous application globally including Mexico, United States and Nepal; indicated for relieving ovarian and uterine pains, easing dysmenorrhea, pregnancy pains, cramp-like pains, spasmodic dysmenorrhea and congestive dysmenorrhea; plant medicine of the West and traditional American Indian use in herbal formulas for childbirth pain, rheumatism, colic and gallbladder problems; herbal actions include anti-inflammatory, antispasmodic, nervine and autonomic nervous system-relaxant effects
Tincture Preparation
Cramp Bark: tincture dosage 4-8 ml, TID (1:5 in 40%), BHP 5 to 10 ml tincture (1:5 in 45%) TID
Corydalis: tincture dosage 1.5 – 2.5 ml TID recommended by David Winston, 5-20 ml recommended by Dr. Aviva Romm
Black Cohosh: tincture dosage 2 to 4 ml TID (1:5 in 60%), BPC 1.8 to 3.6 ml (1:10 in 60%) (Hoffman, 2003); 2-4 ml TID (1:10)
Wild Yam: tincture dosage is 2 to 4 ml TID (1:5 in 40%), BHP 2 to 10 ml tincture (1:5 in 45%) TID; 2-10 ml TID (1:5)
Safety Considerations & Contraindications
Cramp Bark: no reported side effects or drug interactions
Corydalis: contraindicated in pregnancy unless under the supervision of a healthcare practitioner
Black Cohosh: contraindicated during pregnancy except during birth, unless under the supervision of a qualified healthcare practitioner
Wild Yam: no reported side effects or drug interactions
While PMS is quite debilitating for female reproductive health, this condition can be positively supported through a wide variety of herbal medicinal applications. Targeted herbal actions of high therapeutic relevance include hormonal normalizers, uterine tonics, emmenagogues, uterine demulcents, antispasmodics, uterine astringents, hepatics, yin tonics, nervines and anti-inflammatories. The most caution should be exercised with use and dosage during pregnancy. The aforementioned actions are highly beneficial and clinically indicated to support natural fertility, so with proper clinical guidance they can be safely applied to optimize chances of healthy conception.
Wherever you may be on your journey toward optimal health and well-being, I hope you know that there are a wide variety of incredibly potent and helpful herbs with longstanding clinical use to safely consider integrating into your lifestyle. They can help you to feel at your level best and balance the debilitating effects of PMS. From my heart to yours, I wish you the very best of health, hormonal balance and healing!
In health, peace and gratitude,
Whitney
References
Balch, P. A. (2010). Prescription for nutritional healing. Penguin Group.
Bone, K., & Mills, S. (2013). Principles and practice of phytotherapy. Elsevier Ltd.
Braun, L., & Cohen, M. (2015). Herbs and natural supplements: An evidence-based guide volume 2. Elsevier Australia.
Cleveland Clinic. (2022, June 4). Amenorrhea. https://my.clevelandclinic.org/health/diseases/3924-amenorrhea
Easley, T., & Horne, S. (2016). The modern herbal dispensatory: A medicine making guide. North Atlantic Books.
Estés, C. P. (1992). Women who run with the wolves: Myths and stories of the wild woman archetype. Ballantine Books.
Frawley, D. (2000). Ayurvedic healing: A comprehensive guide. Lotus Press.
Gardner, Zoe & McGuffin, M. (2013). American Herbal Products Association’s Botanical Safety Handbook. CRC Press.
Garrett, J. T. (2003). The Cherokee herbal: Native plant medicine from the four directions. Bear & Company.
Hobbs, C. (2016). Herbal action categories. https://www.christopherhobbs.com/webdocs/classhandouts/keville-hobbs-2016/Herbal-Actions.pdf
Hoffman, D. (2003). Medical herbalism: The science and practice of herbal medicine. Healing Arts Press.
Johns Hopkins Medicine. (2022, June 4). Dysmenorrhea. https://www.hopkinsmedicine.org/health/conditions-and-diseases/dysmenorrhea
Kapit, W., Macey, R. I., & Meisami, E. The physiology coloring book. HarperCollins College Publishers.
Lad, V. (1999). The complete book of Ayurvedic home remedies: Based on the timeless wisdom of India's 5,000-year-old medical system. Harmony.
Local Immunity-Boosting Echinacea
Echinacea spp. is a gorgeous native plant found in diverse abundance and multiple unique species across central and southern North America.
Have you experienced this herbal medicine gem?
Echinacea spp. is a gorgeous native plant found in diverse abundance and multiple unique species across central and southern North America. I’ve spent many happy hours gardening in breathtakingly beautiful fields of echinacea and planting new seedlings when working for a native gardening company. This is a staple plant in my home garden as well as our Four Seasons Harmony apothecary!
This powerful immune-enhancing herb is indicated for supporting a variety of specific health conditions, like otitis and rhinitis. Echinacea is helpful for ridding the body of microbial infections by both preventing and repairing tissue caused by infection and acts synergistically when combined with other herbs. Longstanding Indigenous applications include pain relief for burns and neck tension, antidotes for poisonous conditions, cough remedies, reducing fevers and migraine treatment. The flower essence holds the ability to provide dynamic support and vitality for the immune system.
Herbal actions include:
Antimicrobial
Immunomodulator
Lymphatic adaptogenic
Vulnerary
Alterative
Anticancer
Anticatarrhal
Anti-inflammatory
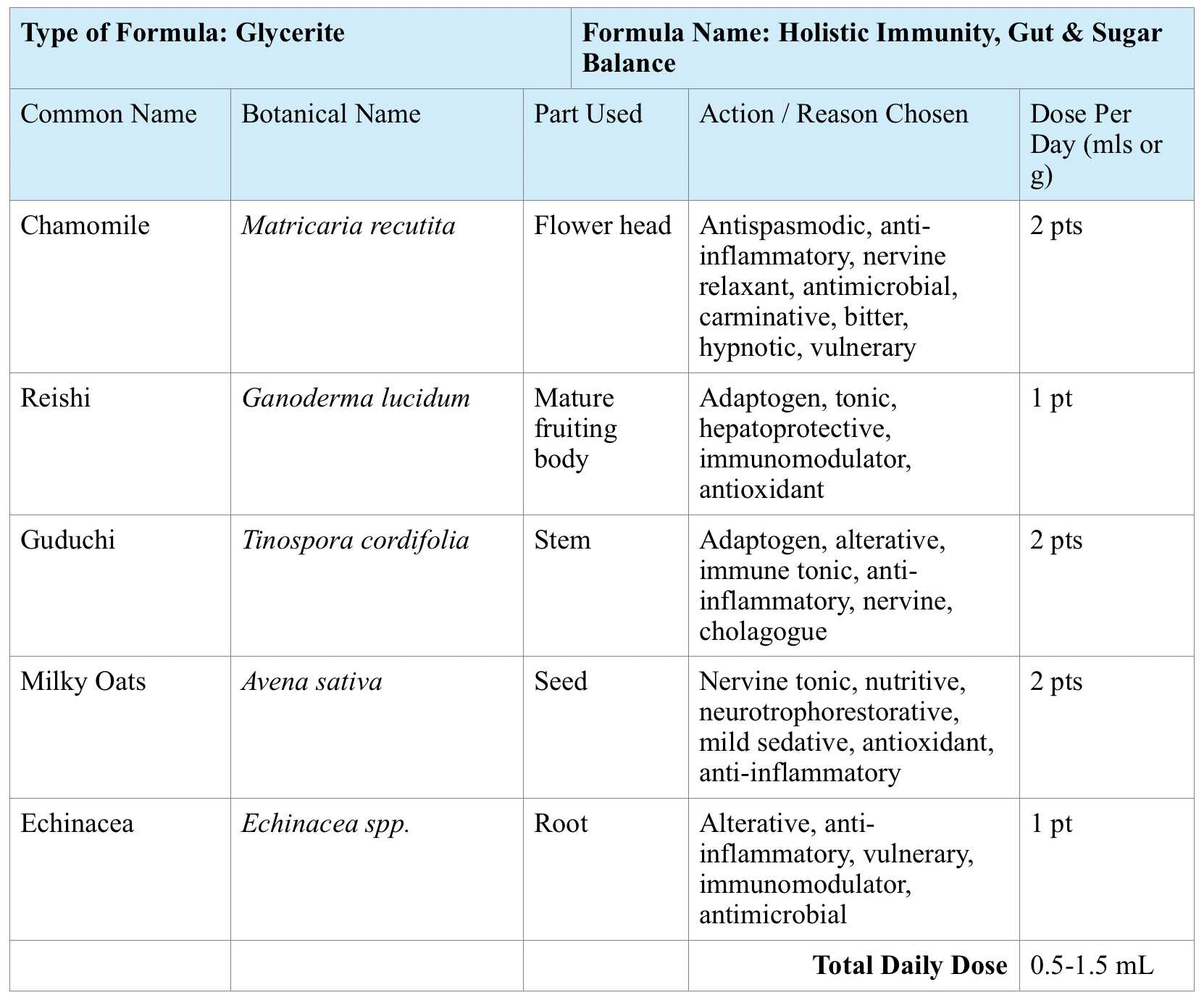
Here is a sample pediatric formula with echinacea that I created to especially support Diabetes I and low immunity:
Initial Pediatric Dosage: Take 0.5 mL or about 1/2 of a droppers full twice a day, ideally 15 minutes away from meals, other herbs and/or supplements mixed into 4-8 oz. of milk, tea, juice, or water as needed. Add favorite milk and whole sweeteners to taste as needed, such as maple syrup, raw honey, stevia or monk fruit.
Additional herbs to consider for Type 1 Diabetes from a promising body of growing evidence-based research include artichoke, bilberry, fenugreek, galangal, gymnema, holy basil (tulsi), and mulberry.
Here is another original formula with echinacea that I created for a woman with breast cancer:
A few other initial dietary recommendations were to ensure that all salt intake is sourced from unrefined sea salt, such as Celtic or Himalayan brands, increase natural electrolytes and trace minerals, cook with more cinnamon and intake molecularly distilled fish or vegan algae oils rich in Omega-3 fatty acids.
Safety: very safe for pregnancy and breastfeeding.
Always ensure that only sustainability harvested, pesticide-free herbs are used. Take care to avoid overharvesting echinacea in the wild, as this is an "at risk" herb. Honor sustainable wild harvesting measures and only take from a truly abundant source. If you are a gardener and live in southern or central North America, consider planting this beauty as it can prolifically at your home as a hearty perennial.
I like to carry a homemade echinacea tincture when traveling to apply as a topical vulnerary in the unforeseen occurrence of a minor scrape, burn, sting or skin rash. This is a wonderful choice to include in your herbal first aid kit for both internal and external application. Please let me know other favorite ways you may enjoy this beauty’s healing gifts!
In health, peace, and gratitude,
Whitney
References
Bone, K., & Mills, S. (2013). Principles and practice of phytotherapy. Elsevier Ltd.
Braun, L., & Cohen, M. (2015). Herbs and natural supplements: An evidence-based guide volume 2. Elsevier Australia.
Easley, T., & Horne, S. (2016). The modern herbal dispensatory: A medicine making guide. North Atlantic Books.
Freeman, Camille. (2020). Pregnancy-friendly herbs. Bloom and Grow Nutrition, LLC.
Hobbs, C. (2016). Herbal action categories. https://www.christopherhobbs.com/webdocs/classhandouts/keville-hobbs-2016/Herbal-Actions.pdf
Hoffman, D. (2003). Medical herbalism: The science and practice of herbal medicine. Healing Arts Press.
Vickery, N. (2012). Re-engaging our senses: Taste. The Family Herbalist. https://thefamilyherbalist.files.wordpress.com/2012/09/herbal-taste-chart.pdf
Williamson, E. M. (2003). Potter’s herbal cyclopaedia. The C. W. Daniel Company Limited.
Relieve Insomnia, Anxiety, Stress & More with Passionflower Herb
Several of passionflower’s herbal indications include relieving insomnia, anxiety, pain, irritability with difficulty falling asleep, palpitations, lowering blood pressure, nervous restlessness, tenseness, seizures and stress.
Passionflower, an Herbal Medicine Powerhouse
I first met stunning passionflower as an eighteen-year-old working on an organic farm overlooking the Tasman Sea in spectacular Punakaiki, West Coast, New Zealand. Growing abundantly in lush, overflowing, unmistakable violet vines, the fruit was harvested as a delicious, nutritious edible and celebrated as an herbal medicine star. To this day, I love being in the garden with gorgeous passionflower!
What makes this plant so unique? Several of passionflower’s herbal indications include relieving insomnia, anxiety, pain, irritability with difficulty falling asleep, palpitations, lowering blood pressure, nervous restlessness, tenseness, seizures and stress.
Passionflower, Passiflora incarnata, is a native plant in North, Central and South America. Along with all medicinal native plants, passionflower has been safely applied for thousands of years amongst Indigenous people. For example, the Cherokee include passionflower roots in various medicinal preparations as a dermatological aid, gastrointestinal balance, ear medicine, liver support and pediatric aid. The Houma traditionally apply an infusion of the roots as a blood tonic.
Throughout the entirety of my clinical healthcare practice, I have heavily recommended passionflower as a stand-alone herb as well as blended into custom formulas. I continue to see a huge need for this beauty’s healing gifts to restore health, balance and well-being. There is a significant growing body of research on passionflower’s support for anxiety symptoms, including pre-surgery anxiety, since it is gentle without interacting with general anesthesia. When combined with St. John’s Wort, Hypericum perforatum, the duo assists in relieving depression with anxiety.
I often recommend passionflower during intense times because this plant is incredibly safe with no known contraindications. Passionflower embodies cooling, relaxing, astringent and pungent energetics. The flower essence can be applied toward feeling a deep sense of safety, support in the path toward self-realization and releasing muscular tension. Additionally, passionflower is indicated for helping with drug withdrawal symptoms.
Safety and contraindications: there are no known safety or drug-herbal interaction concerns. Passionflower is considered extremely safe for general use, as well as pregnancy and lactation.
The fruit is a delicious edible and can be eaten raw, crushed into juice or prepared in other lovely ways. The young shoots and leaves are also edible, such as combined with other greens in a salad or cooked in a vegetable sauté.
I hope you enjoy radiant passionflower’s many gifts!
Cheers to your highest health and well-being,
Whitney
References
American Botanical Council. (2000). Excerpt from Herbal Medicine: Expanded Commission E Monographs. Integrative Medicine Commissions.
http://cms.herbalgram.org/expandedE/Willowbark.html
Gardner, Zoe & McGuffin, M. (2013). American Herbal Products Association’s Botanical Safety Handbook. CRC Press.
Garrett, J. T. (2003). The Cherokee herbal: Native plant medicine from the four directions. Bear & Company.
Hoffman, D. (2003). Medical herbalism: The science and practice of herbal medicine. Healing Arts Press.
Moerman, D. E. (2009). Native American medicinal plants: An ethnobotanical dictionary. Timber Press.
Therapeutic Research Center. (2020, November 16). Passionflower. Natural Medicines Database. https://0-naturalmedicines-therapeuticresearch-com.sclcatalog.muih.edu/databases/food,-herbs-supplements/professional.aspx?productid=871
Postpartum Ceremony to Nourish New Mothers
Holding sacred space for another local postpartum mother and her family to receive a Closing of the Bones ceremony is such a deep gift. Pregnancy and birth expand the mother's physical body and energy field significantly to usher in new human life.
Closing of the Bones Ceremony
Holding sacred space for another local postpartum mother and her family to receive a Closing of the Bones ceremony is such a deep gift. Associated with a Mexican postpartum tradition, it is also referred to as Cerrar la Cadera or La Cerrada. Pregnancy and birth expand the mother's physical body and energy field significantly to usher in new human life. Hence, one of the core aspects in many traditional postpartum care practices involves helping to “close" women up.
Several of the many physiological expansions during pregnancy include:
Increases in the hormone relaxin
Blood volume increases by on average of 50%
Diastasis recti expansion in 100% of women
Pelvic opening during birth to allow for the baby's passage
Emotional, psychological and spiritual expansions are numerous as well and unique to each mother.
The cross-cultural La Cerrada practice is a powerful way to aid in closing the mother’s physical, emotional, spiritual and mental bodies so she can reconnect with herself and be fully present.
Benefits include:
Abdominal work to help bring the fascia and muscles closer together for more effective pelvic floor and core contractions
A break for deep rest, self-care and nourishment
Facilitate the important process of closing the pelvis after birth
Sharing the mother’s birth story
Giving a closing ceremony with family and friends
Closing of the Bones is included in my Postpartum package around forty-two days after birth to mark closing the mother’s sacred window, or whenever she feels ready. Doing this three times during the mother’s sacred window is normal in Mexican midwifery traditions. It’s also very beautiful to receive years later.
If you’re interested to learn more, please contact me to schedule a complimentary Breakthrough Session at www.fourseasonsharmony.com/classesandprograms.
I hold much gratitude to my teachers for exquisitely sharing these teachings and the lineages holding profound maternal care, knowledge and wisdom.
In gratitude, love and service,
Whitney
Reference
Soma-Shakti School of Women's Vedic Wisdom. (2022). Soma-Shakti Ayurvedic Postpartum Treatment Training. Soma-Shakti Australia.
How to Make Elderberry Syrup
Homemade elderberry syrup is a top personal go-to year-round for immunity boosting. The multitude of healing benefits of the renowned Elder tree date back millennia in many traditional cultures.
Boost Your Immunity with Homemade Elderberry Syrup
Homemade elderberry syrup is a top personal go-to year-round for immunity boosting. I especially lean on this powerful DIY medicine for staying healthy amidst freezing winter temperatures. The multitude of healing benefits of the renowned Elder tree date back millennia in many traditional cultures. Please enjoy one of my favorite recipes that you can also share with family and friends!
Ingredients
2 cups dried elderberries
4 cups water
1 cup raw, sustainably harvested honey
3-4 cinnamon sticks
½ - 1 Tbsp grated lemon peel
¼ oz cloves or star anise
¼ - ½ cup elderflower brandy (optional)
Directions:
1. Bring the water and berries to a boil, reduce the heat and simmer for 45 minutes
2. Smash the berries and strain through a muslin cloth
3. Return the syrup to the stove, add the spices and lemon peel, and simmer for an additional 15 minutes
4. Strain, stir in the honey when 110 degrees or less and allow to cool before bottling
Herbal Actions of Elderberry, Sambucus nigra, S. canadensis:
Anti-inflammatory
Antioxidant
Antirheumatic
Antiviral
Decongestant
Diaphoretic
Diuretic
Immunomodulator
Mild laxative
Nutritive
Contraindications: avoid eating raw elderberries; when cooked, the berries are extremely safe for adults, children and breastfeeding mothers.
The sustainably sourced, high quality, delicious local raw honey that I used in this recipe is from friends at The Blackberry Herbarium in Harrisonburg, Virginia.
The gorgeous white flowers of the elder tree are also incredibly medicinal. Children love to eat, decorate and play with them! I hope you enjoy the multitude of healing applications gifted by the elder tree.
In health, peace and gratitude,
Whitney
References
Easley, T., & Horne, S. (2016). The modern herbal dispensatory: A medicine making guide. North Atlantic Books.
Gardner, Zoe & McGuffin, M. (2013). American Herbal Products Association’s Botanical Safety Handbook. CRC Press.
Hoffman, D. (2003). Medical herbalism: The science and practice of herbal medicine. Healing Arts Press.
Milagro School of Herbal Medicine. (2021). Elder. https://www.milagroschoolofherbalmedicine.com/materia-medica.html
Moerman, D. E. (2009). Native American medicinal plants: An ethnobotanical dictionary. Timber Press.
Williamson, E. M. (2003). Potter’s herbal cyclopaedia. The C. W. Daniel Company Limited.
Nature’s First Aspirin: Pain-Relieving White Willow Bark
Seeing a beautiful willow tree and its swaying branches as seemingly vulnerable while actually quite strong inspires feelings of strength, hope, peace, reflection, and wonder.
A Featured Herbal Medicine in Four Seasons Harmony Apothecary
The white willow tree, Salix alba, dates back in medicine to being the original form of aspirin, most especially through its renowned anti-inflammatory salicylic acid chemical constituent. This tree has always struck me as gorgeous with an unusual shape. Seeing a beautiful willow tree and its swaying branches as seemingly vulnerable while actually quite strong inspires feelings of strength, hope, peace, reflection, and wonder.
Clients often ask about natural sources of pain relief and there is extensive research showing this extraordinary’s herb capacity to reduce inflammation. White willow’s herbal actions include functioning as a whole plant medicine analgesic, anti-inflammatory, and tonic. Post-surgery pain recovery, headaches, PMS, and sensitive digestive systems that cannot tolerate NSAIDS are several general, common reasons that I’ve noticed inspire regular interest in a natural form of pain relief without negative side effects. I have seen white willow bark included in many herbal analgesic blends on the market, and love to include this profound herb into customized clinical herbal formulas carefully created by hand in our Four Seasons Harmony apothercary.
Aspirin or acetylsalicylic acid is a synthetic elaboration of the whole plant chemical compound of salicylic acid found in white willow bark, Salix spp., and meadowsweet, Filipendula ulmaria (Ganora, 2009). This over-the-counter nonsteroidal anti-inflammatory drug (NSAID) is commonly used for relief of mild to moderate pain, swelling and inflammation. The potential dangers posed by aspirin can lead to issues like stomach ulcers, hemorrhaging and gastric irritation is reflective only of synthetic salicylates, but not the whole form of salicylate-containing herbs such as meadowsweet or willow bark (Hoffman, 2003; Bone & Mills, 2013).
There are fascinating references of white willow being applied in Romania for ethnopediatry, where it has been traditionally used in Romanian folk medicine to treat child epilepsy (Petran et al., 2020). White willow is regarded as applicable in antiseptic, astringent, fever, malaria, and rheumatism in Turkey, as well as for malaria in Spain and an astringent and callus across Europe (Duke, 1992). Parts of the plant used include in herbal medicine include the leaf, bark, wood, stem, pollen, folium, stem bark, wood, root and spore (Duke, 1992; Royal Botanic Gardens, n.d.). This tree’s habitat includes “wet soils of stream banks and valleys near cities (Little, 1980, p. 328).”
-Whitney Erwin, MSc, MEd, LMT, owner and clinical herbalist at Four Seasons Harmony
References
Bone, K., & Mills, S. (2013). Principles and practice of phytotherapy. Elsevier Ltd.
Duke, James A. 1992. Handbook of phytochemical constituents of GRAS herbs and other economic plants. Boca Raton, FL: CRC Press. Retrieved from: https://phytochem.nal.usda.gov/phytochem/plants/show/1739qlookup=willow&offset=0&max=20&et=
Ganora, L. (2009). Herbal constituents: Foundations of phytochemistry. Herbalchem Press.
Hoffman, D. (2003). Medical herbalism: The science and practice of herbal medicine. Rochester, VT: Healing Arts Press.
Little, E. (1980). National audubon society field guide to north american trees. New York, NY: Alfred A. Knopf.
Moerman, Daniel. (2009). Native American medicinal plants. Portland, OR: Timber Press, Inc. United States Department of Agriculture. (2019). Salix alba L. white willow. Retrieved from: https://plants.usda.gov/core/profile?symbol=SAAL2
Petran, M., Dragos, D. & Gilca, M. (2020). Historical ethnobotanical review of medicinal plants used to treat children diseases in Romania (1860s–1970s). J Ethnobiology Ethnomedicine 16, Article 15. https://doi.org/10.1186/s13002-020-00364-6
Ayurveda for Summer Balance
Ayurveda, the art of living daily in harmony with nature, is the mother to all of the world’s healing systems.
Tropic like it's hot! As the solar energy builds significantly at the end of the spring season, fire qualities start to accumulate as we transition into the pitta predominant season of summer with more hot, sharp and bright qualities. A major seasonal change can affect our mind, bodies and spirits into either further balance or imbalance depending on how we respond. How are you feeling with the intense solar heat of summer accumulating for those who live in the northern hemisphere? Are you in seventh heaven, struggling immensely or somewhere in between? Wherever you may fall on this spectrum, this tends to be a reflection of each of our unique constitutions and can vary dramatically from person to person.
I acknowledge with humble gratitude how the profundity of holistic tools support staying at each unique person's level best and love to share this knowledge outwardly with others, too. Ayurveda recognizes that our health is significantly influenced by our unique, individual constitution, as well as external factors such as the changing of the seasons throughout the year. Understanding how to best make decisions in balance with the rhythms of nature through the ideas of Ayurveda can greatly improve our ability to heal, quality of life, productivity, and longevity. So, what do we do to take care of ourselves to get through the summer months with grace, health, and fulfillment?
Pitta is composed of fire and water elements and is responsible for transformation and metabolism in the body. The healing energy of pitta can be balanced with cooling foods, less intense exercise, protection from the heat of the midday sun and softening intense schedules to stay at our level best.
PITTA BALANCING LIFESTYLE RECOMMENDATIONS FOR SUMMER INCLUDE:
* Self-massage (Abhyanga) before taking a shower or bath with a cooling oil such as coconut or sunflower to calm the nervous system and cool the body
* On hot days, resting, a short nap and/or yoga nidra can be restorative
* Cultivate calm inner awareness
* Dress in light, breathable clothing and cooling colors such as blue, green, white and lavender
* Ideally, exercise by breathing through your nose and to 50-70% of your capacity
* Avoid exercising between 10 am - 2 pm, a high pitta time of day
* Favor the essential oils of Lavender, Jasmine, Vetiver and Rose Geranium
* Wash, dry and massage feet with a plain or herbal oil at bedtime
* Wear a wide-brimmed hat and sunglasses outdoors to shelter from the sun
Here is a general overview of foods to concentrate on to balance pitta:
Fruits to Favor:
Apples
Avocados
Berries
Cherries
Coconut
Cranberries
Grapes
Limes
Mangoes
Melons
Pears
Pineapples
Plums
Pomegranates
Prunes
Vegetables to Favor:
Artichokes
Asparagus
Beet Greens
Broccoli
Brussel Sprouts
Cabbage
Cauliflower
Celery
Chard
Collard Greens
Cucumbers
Green Beans
Kale
Lettuce
Okra
Potatoes
Watercress
Zucchini
Grains to Favor:
Barley
Rice, Basmati
Wheat
Legumes to Favor:
Adzuki Beans
Black Beans
Garbanzo Beans
Mung Beans
Soy Beans & Products (always fermented)
Split Peas
Oils to Favor:
Coconut Oil
Olive Oil
Sunflower Oil
Spices and Garnishes to Favor:
Basil
Cardamom
Cilantro
Coriander
Dill
Fennel
Lime
Mint
Parsley
Animal Products to Favor (If You Eat Them):
Fish (freshwater)
Poultry (white)
Shrimp
Sweeteners:
Maple Syrup
Unrefined Cane Sugar
Turbinado
Check out our Summer Seasonal Recipes webpage for recipe ideas! Wishing you and your families vibrant health, happiness, and longevity!
-Whitney Erwin, MSc, MEd, LMT, owner of Four Seasons Harmony
Resilience, Hormesis, Xenohormesis & Adaptation
The growing organic and wild harvested movements seem to be a culturally adaptive protection of healthy food sources that can create a different trajectory for human health amidst the explosion of agrochemicals very recently in modern history.
Resilience
Ever wondered how to navigate the numerous challenges that we face as humans with greater strength, resilience, and knowledge? Here we explore the back story on important scientific terms that we apply all of the time in clinical practice, such as recommending diversity of phytochemicals in the diet and how to balance safe dosing for unique constitutional needs. Resilience is the ability of a biological organism on a micro or macro scale, such as an animal or interdependent ecosystem like wetlands, to defend and recover from an environmental disturbance or change. To what degree the process of resilience can be strengthened or weakened depends on a multitude of factors influencing the overall functioning of the organism. For example, you can increase resilience by intaking herbal medicine like adaptogens to help your entire body more effectively resist stress.
Hormesis
Hormesis is a complex scientific concept relating to how exposure to a chemical or biological substance and whether it has the effect of being beneficial or detrimental depends on its quantity. This idea reflects a nuanced complexity of how the amount and context of a substance can have either a medicinal or poisonous effect, while not inherently defined as having only one of these actions. For example, a smaller amount of a vitamin such as fat-soluble D could be healing toward an organism, though if given in a larger amount could be dangerous and toxic. The concept of hermetic properties extends to lifestyle choices on physiology, such as in reference to moderate exercise or calorie restriction “being harmful at high doses yet beneficial at relevantly low doses” (Son et al., 2009).
An example of hormesis is in choosing the dosage of a medicinal plant and how it impacts a human toward healing or disease. For example, the renowned turmeric root from oral accounts of my Ayurvedic teachers is very normal to intake daily in India and a major reason that Indians exhibit less neurological problems. The medicinal application of turmeric when given up to approximately 15,000 mg contains zero contraindications or negative side effects with amazing benefits to human health and increased phytochemical intake (Pole, 2012).
Xenohormesis
Xenohormesis is specific hormetic concept relates to the external sensory perception and communication between organisms impacting them biologically when there is a change in one of these interdependent relationships (Tims, n.d.). For example, Baur et al. (2008) describes how “polyphenols such as resveratrol and quercetin, which are produced by stressed plants, activate sirtuin enzymes and extend the lifespan of fungi and animals.” Botanical chemical changes that fluctuate under stress are an inherent protective mechanism that may be either beneficial or harmful depending on the context, such as in the latter case of increasing longevity for animals and fungi dependent on specific plants to survive within the same ecosystem. Xenohormesis is an adaptive response “in the physiology of an organism to molecular cues that are neither nutritive nor direct stressors” and give us fascinating insight into the ever-changing dynamics between life forms.
Adaptation
Adaptation is the capability of a species, culture, or ecological system to change to meet evolving characteristics that influence survival such as environment, food sources, gene mutations, and exposure to the elements to sustain life and endure. The changes necessitate flexibility and result in new and ever-evolving expressions as needed to survive.
One example of adaptation is in the growing research and observations on the impact of human health related to the modern treatment of agrochemicals such as commercial Roundup. Human beings that are exposed to these toxins can experience negative biological reactions, such as increasing the risk of infertility, which is changing the livelihood and cellular makeup of both plants and humans. The growing organic and wild harvested movements seem to be a culturally adaptive protection of healthy food sources that can create a different trajectory for human health amidst the explosion of agrochemicals very recently in modern history. Also, cross-pollination of organic foods by GMO crops is forcing plants to adapt to exposure as well as inspiring human actions to protect and create native seed banks.
By increasing consumption of wild plants or local organic seasonal foods and herbs, one’s diet would be diversified with more phytochemicals (Tims, n.d.). The benefit of increasing one’s exposure to phytochemicals would increase the chances of resistance to disease, stress, and environmental fluctuations because the person would literally have a wider span of potential to activate hormetic pathways and effect positive, small cellular stress responses (Son et al., 2009). The plethora of specific phytochemicals that have been extensively researched demonstrate greater resilience through preventive medicine, decreasing the chances of illness such as cancer, Alzheimer’s disease and autoimmune disease. Examples include the benefits of consuming green tea’s polyphenolic compounds to reduce inflammation and the risk of coronary artery disease, as well as sulforaphane in broccoli sprouts and cruciferous vegetables which “protect cultured neurons against oxidative stress and dopaminergic neurons against mitochondrial toxins” (Son et al., 2009).
-Whitney Erwin, MSc, MEd, LMT, owner of Four Seasons Harmony
References
Baur, J.A. & Sinclair, D. A. (2008). What is Xenohormesis? Am J Pharmacol Toxicol. 3(1):152-159. https://pubmed.ncbi.nlm.nih.gov/26949380/
Pole, S. (2012). Ayurvedic medicine: The principles of traditional medicine (1st ed.). Singing Dragon.
Son, T.G., Camandola, S., & Mattson, M. (2009). Hormetic Dietary Phytochemicals. Neuromolecular Med. 2008; 10(4): 236-246. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2635914/
Tims, M. (n.d.). Co-evolution of humans and plants [Online Lecture]. Retrieved from Maryland University of Integrative Health graduate course materials.